Small bowel perforation due to a blunt abdominal trauma with inguinal herniation accompanied by an acute sigma diverticulitis: a case report
Written by Lukas W. Widmer
Category
Published 15 December 2017

Small bowel perforation due to a blunt abdominal trauma with inguinal herniation accompanied by an acute sigma diverticulitis: a case report
Lukas W. Widmer MD, Michael Müller MD
Department of General Surgery and Orthopedics, Hospital Davos, Switzerland
Introduction
Although small bowel injuries are the most frequent hollow viscus injuries in blunt abdominal trauma they occur with a low incidence of 1.2% [1,2]. Inguinal hernias are frequent and a watchful waiting approach in asymptomatic male patients is safe and advised in older men or in the presence of major comorbidities [3]. However, long-term follow-up of observation groups showed a high conversion rate to surgery of up to 70% after 7.5 to 10 years [4,5]. Increased pain was the most common reason for a crossover to surgery. An incarceration was only causative in 2% of the cases. Surgical treatment is recommended urgently in case of a strangulation and should be performed electively in symptomatic inguinal hernias with the open Lichtenstein or an endoscopic mesh technique [6].
Compared to that, the progression of incidental diverticulosis found during colonoscopy to an acute diverticulitis was uncommon [7]. In the median 7-year follow-up of 2’222 patients, only 4% developed acute diverticulitis. A traumatic intestinal perforation in association with an inguinal hernia is a rare condition which has been reported as early as 1937 [8]. We report the case of a small bowel perforation due to a blunt abdominal trauma with a concomitant acute sigma diverticulitis in a 74-year old male with a left-sided inguinal hernia.
Case report
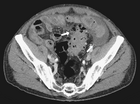
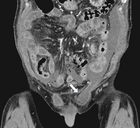
A physically fit 74-year old male with a known history of a left-sided inguinal hernia presented to our emergency department with lower abdominal pain after a fall while playing tennis. After striking the ball the patient fell forward, landed on both his hands and suffered a blunt trauma to his abdomen. He identified a swelling in the left groin and reduced the content back into the abdomen. Due to persisting pain in the lower abdomen he presented to our emergency department. The vital signs were normal and the examination showed tenderness in the lower abdomen without signs of peritonitis. No evidence of incarceration of the inguinal hernia was present. The white blood cell (WBC) count was 13’000 and the c-reactive protein was 17mg/l. The abdominal sonography showed no free fluid or air and the patient was hospitalized for analgesic treatment. Thereby the patient was free of symptoms on the following day. On the second day after the injury the condition of the patient worsened with vomiting and a ballooned abdomen. An erect x-ray of the chest showed free intraabdominal air (Figure 1). The labs showed a WBC count of 6’000, a c-reactive protein of 463mg/l, a creatinine of 136umol/l and normal liver enzymes and lipase. The computed tomography (CT) of the chest and abdomen with intravenous contrast
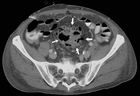
showed considerable free fluid, free air and a thickened wall of the sigma with multiple diverticula imposing as a pseudotumor without signs of an acute inflammation (Figure 2). This rose the suspicion of a traumatic sigma perforation. The left inguinal canal was fluid-filled with free air present (Figure 3). Because of the absence of an intensive care unit the patient was transported to a tertiary referral hospital for an urgent explorative laparotomy. The inspection showed a feculent 4-quadrant peritonitis with a perforation of the small bowel 50cm proximal to the ileocecal valve. The perforated small bowel was resected as a segment. A side-to-side ileostomy was formed. The sigma was indurated on palpation and suspicious of a colon cancer. In the intraoperative rectoscopy the tumor could not be reached. The inguinal canal was filled with stool and a lavage was performed together with the whole abdomen. A drainage was placed and the abdomen closed temporary with a negative-wound-pressure therapy (NWPT) system. The preoperatively started intravenous antibiotic treatment with imipenem was continued. On the first postoperative day, a rectosigmoidoscopy was unable to pass the stenosis in the sigma. A repeat CT of the abdomen with rectal and intravenous contrast showed wall thickening of the sigma with perifocal lymphadenopathy (Figure 4). In the 2nd look laparotomy 48 hours after the initial operation an anterior resection with complete mesocolic excision and partial mesorectal excision was performed because a malignant disease could not be excluded. A descendorectostomy was performed and the side-to-side ileostomy was reversed into a protective splitstoma. Again, the inguinal hernia was not touched due to the contamination. The NWPT was continued and after two NWPT changes primary fascial closure was achieved eleven days later. The histopathology showed a covered perforation of a sigma diverticulitis with inflamed pseudotumor without signs of malignancy. 22 days after the tennis accident the patient was discharged for rehabilitation. One month later he is in a good health condition and is waiting for the reversal of the stoma and definitive treatment of the inguinal hernia.
Discussion
Hollow viscus injuries (HVI) occur in only 1% of all blunt trauma admissions and affect most often the small bowel [1]. Despite the low incidence HVI are associated with a high mortality rate and in patient with an isolated small bowel perforation the time to operative intervention significantly increased mortality. The low incidence and the increasing mortality with time to operative intervention in patients with a blunt HVI was confirmed in another study [2]. The authors demonstrated that a high percentage of the deaths in the groups with a delay in operative therapy was due to abdominal-related sepsis and multiple organ failure. The diagnostic approach to a stable patient with a blunt abdominal trauma is challenging. The Focused Assessment with Sonography in Trauma (FAST) examination seems not sensitive enough to rule out intraabdominal injuries. Sensitivity has been described to be only between 22% and 41% in hemodynamically stable blunt abdominal trauma patients [9,10]. This lack of sensitivity is also integrated in the EAST practice management guidelines for blunt abdominal trauma, which suggest to follow-up a negative FAST with a repeat sonography, observation or a CT scan [11]. This lack of sensitivity of abdominal sonography in blunt trauma is reflected in our case report where the patient was observed after a negative FAST exam. On the contrary, an admission or observation is not necessary after a negative abdominal CT scan, especially if the patient is asymptomatic [12,13]. But up to 13% of patients with a small intestinal perforation after blunt trauma have a normal abdominal CT scan [14].
Incarceration and strangulation are feared complications of a watchful waiting strategy in inguinal hernias. An intestinal perforation due to blunt abdominal trauma in patient with inguinal hernias is a rare condition. But the association has been made as early as 1937 by Aird from Edinburgh [8]. A larger case series was reported by Payson and Mage including eight patients [15]. They summarize three mechanisms of injury. First, the perforation occurring at the internal inguinal ring due to difference in pressure between the abdominal cavity and the inguinal canal. Second, the perforation happens inside the inguinal canal in a reducible hernia due to pressure differences. After muscle relaxation, the perforated loop slips back into the abdominal cavity. And thirdly, if the intestine is fixed within the abdominal cavity and the sudden increase of pressure resulting in a shearing injury with the perforation happening inside the abdominal cavity. In our case, we believe the second mechanism of injury to be the reason for the perforation because of the history of the patient with the self-reduction of the herniation after the injury. We did not find any case report of a traumatic small intestinal perforation in a patient with inguinal hernia occurring concomitant with an acute sigma diverticulitis. Due to the two-day delay in the diagnosis of the small bowel perforation a fecal fluid collection may have formed in the pelvis, which led to the inflammation around the sigma. The diagnosis was initially missed due to the good general health condition of the patient with little pain and no signs of peritonitis or fever. The prevalence of large bowel diverticulosis is as high as 23-29% in autopsy and double contrast barium enema studies from Greece and Thailand [16]. The rate of colonic diverticulosis found incidentally in routine colonoscopy is increasing over time and with patient age [17].
A recent Danish database study linked colonic diverticulosis to direct inguinal hernia repair [18]. In 13’855 patients, the prevalence of large bowel diverticulosis was 26% and this was associated with direct inguinal hernia repair with an odds ratio of 1.3 (95% confidence interval 1.0-1.8). A possible explanation might be the herniosis hypothesis, which assumes a systemic connective tissue disease being at the core of both diseases.
Admission rates for acute diverticulitis increased from 1998 on in the United States with an estimated rate of admission of 0.7 per 1000 population in 2005 [19]. In the same period the rate of admitted patients undergoing urgent surgery decreased from 17 to 14%. In Switzerland the incidence of hospitalization due to acute uncomplicated diverticulitis rose in the period 2004-2011 to 85 per 100’000 inhabitants [20]. In this period, the incidence of colon resections for uncomplicated diverticulitis dropped, but on multivariable analysis the probability of a resection for hospitalized patients increased. This trend is opposite to recent guidelines, which opt for an individualized decision on when to perform an elective resection based on patient-related factors rather than number of previous episodes of diverticulitis [21,22]. However, in cases of diffuse peritonitis an urgent resection is advised. The decision to perform a Hartmann resection, a primary resection with anastomosis or damage control surgery should be tailored to the hemodynamics and co-morbidities of the patient. In our case an oncologic resection with a protective stoma formation was attempted in the re-laparotomy because an underlying malignancy could not be excluded.
Conclusion
Diverticulosis and inguinal hernia are diseases with a high prevalence and a potential link through a weakness in the connective tissue. Blunt abdominal trauma results in an increase in intraabdominal pressure and the clinician should be vigilant for intraabdominal injuries, especially in cases with a history of acute herniation after the blunt trauma. A negative FAST exam alone is not sufficient to discharge the patient. An acute diverticulitis concomitant to a small bowel perforation is a rarity.
References
[1] Watts DD, Fakhry SM. Incidence of hollow viscus injury in blunt trauma: an analysis from 275,557 trauma admissions from the East multi-institutional trial. J Trauma 2003;54:289–94. doi:10.1097/01.TA.0000046261.06976.6A.
[2] Malinoski DJ, Patel MS, Yakar DO, Green D, Qureshi F, Inaba K, et al. A Diagnostic Delay of 5 Hours Increases the Risk of Death After Blunt Hollow Viscus Injury. J Trauma Inj Infect Crit Care 2010;69:84–7. doi:10.1097/TA.0b013e3181db37f5.
[3] Miserez M, Peeters E, Aufenacker T, Bouillot JL, Campanelli G, Conze J, et al. Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 2014;18:151–63. doi:10.1007/s10029-014-1236-6.
[4] Fitzgibbons RJ, Ramanan B, Arya S, Turner S a, Li X, Gibbs JO, et al. Long-term results of a randomized controlled trial of a nonoperative strategy (watchful waiting) for men with minimally symptomatic inguinal hernias. Ann Surg 2013;258:508–15. doi:10.1097/SLA.0b013e3182a19725.
[5] Chung L, Norrie J, O’Dwyer PJ. Long-term follow-up of patients with a painless inguinal hernia from a randomized clinical trial. Br J Surg 2011;98:596–9. doi:10.1002/bjs.7355.
[6] Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 2009;13:343–403. doi:10.1007/s10029-009-0529-7.
[7] Shahedi K, Fuller G, Bolus R, Cohen E, Vu M, Shah R, et al. Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol 2013;11:1609–13. doi:10.1016/j.cgh.2013.06.020.
[8] Aird I. The association of inguinal hernia with traumatic perforation of the intestine. Br J Surg 1937;24:529–33. doi:10.1002/bjs.1800249510.
[9] Natarajan B, Gupta PK, Cemaj S, Sorensen M, Hatzoudis GI, Forse RA. FAST scan: Is it worth doing in hemodynamically stable blunt trauma patients? Surgery 2010;148:695–701. doi:10.1016/j.surg.2010.07.032.
[10] Carter JW, Falco MH, Chopko MS, Flynn WJ, Wiles CE, Guo WA. Do we really rely on fast for decision-making in the management of blunt abdominal trauma? Injury 2015;46:817–21. doi:10.1016/j.injury.2014.11.023.
[11] Hoff WS, Holevar M, Nagy KK, Patterson L, Young JS, Arrillaga A, et al. Practice management guidelines for the evaluation of blunt abdominal trauma: the East practice management guidelines work group. J Trauma 2002;53:602–15. doi:10.1097/01.TA.0000025413.43206.97.
[12] Livingston DH, Lavery RF, Passannante MR, Skurnick JH, Fabian TC, Fry DE, et al. Admission or observation is not necessary after a negative abdominal computed tomographic scan in patients with suspected blunt abdominal trauma: results of a prospective, multi-institutional trial. J Trauma 1998;44:273-80-2.
[13] Benjamin E, Cho J, Recinos G, Dilektasli E, Lam L, Brunner J, et al. Negative CT can Safely Rule out Clinically Significant Intra-abdominal Injury in the Asymptomatic Patient After Blunt Trauma. J Trauma Acute Care Surg 2017:1. doi:10.1097/TA.0000000000001705.
[14] Fakhry SM, Watts DD, Luchette FA. Current Diagnostic Approaches Lack Sensitivity in the Diagnosis of Perforated Blunt Small Bowel Injury: Analysis from 275,557 Trauma Admissions from the EAST Multi-Institutional HVI Trial. J Trauma Inj Infect Crit Care 2003;54:295–306. doi:10.1097/01.TA.0000046256.80836.AA.
[15] Payson BA, Mage S. Role of Inguinal Hernia in Acute Perforation of the Small Intestine Secondary to Blunt Abdominal Trauma. Ann Surg 1962;156:944–50.
[16] Paspatis GA, Papanikolaou N, Zois E, Michalodimitrakis E. Prevalence of polyps and diverticulosis of the large bowel in the Cretan population. An autopsy study. Int J Colorectal Dis 2001;16:257–61.
[17] Nagata N, Niikura R, Aoki T, Shimbo T, Itoh T, Goda Y, et al. Increase in colonic diverticulosis and diverticular hemorrhage in an aging society: Lessons from a 9-year colonoscopic study of 28,192 patients in Japan. Int J Colorectal Dis 2014;29:379–85. doi:10.1007/s00384-013-1808-4.
[18] Oma E, Jorgensen LN, Meisner S, Henriksen NA. Colonic diverticulosis is associated with abdominal wall hernia. Hernia 2017. doi:10.1007/s10029-017-1598-7.
[19] Etzioni DA, Mack TM, Beart RW, Kaiser AM. Diverticulitis in the United States: 1998–2005. Ann Surg 2009;249:210–7. doi:10.1097/SLA.0b013e3181952888.
[20] von Strauss und Torney M, Thommen S, Dell-Kuster S, Hoffmann H, Rosenthal R, Young J, et al. Surgical treatment of uncomplicated diverticulitis in Switzerland: comparison of population-based data over two time periods. Color Dis 2017;19:840–50. doi:10.1111/codi.13670.
[21] Sartelli M, Catena F, Ansaloni L, Coccolini F, Griffiths EA, Abu-Zidan FM, et al. WSES Guidelines for the management of acute left sided colonic diverticulitis in the emergency setting. World J Emerg Surg 2016;11:37. doi:10.1186/s13017-016-0095-0.
[22] Feingold D, Steele SR, Lee S, Kaiser A, Boushey R, Buie WD, et al. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum 2014;57:284–94. doi:10.1097/DCR.0000000000000075.

Thank you for this interesting case report. This patient is showing that cause and effect or disease are sometimes difficult to connect and different diagnosis can occur simultaneously.