Traumatic Aortic Rupture after a Paragliding Accident
Written by Andreas Kohler
Category
Published 13 April 2014

Andreas Kohler MD, Vladimir Makaloski MD, Beat Schnüriger MD
Department of Visceral and Transplant Surgery, Bern University Hospital, Switzerland
Department of Vascular Surgery, Bern University Hospital, Switzerland
Introduction
We report a case of a covered aortic rupture at the classic location distal to the left subclavian artery. Since this injury is rare and the clinical picture very variable, a high index of suspicion is required. On the basis of this case, we discuss clinical aspects of a blunt aortic rupture and illustrate the therapy by endovascular aortic stenting.
Case
The 39-year-old male patient suffered a crash during paragliding. While performing a helical curve, he hit the ground directly at full speed without having the possibility of preparing a landing.
He was immediately transported to a regional hospital, where the initial assessment, including a contrast enhanced CT scan, was performed. The CT scan revealed a type B pelvic fracture as well as the suspicion of a covered aortic rupture. Therefore the patient was immediately transferred by air ambulance to Bern University Hospital for further management.
On arrival in our trauma bay, the patient was fully alert and orientated. No focal neurologic deficit was present. He was breathing spontaneously; auscultation showed bilateral normal breath sounds and no emphysema or other signs for pneumothorax/haemothorax were noticed. Moreover, no systolic murmur over the precordium or hoarseness was present. Blood pressure was at 105/70 mmHg (after labetalol and fentanyl); the heart rate was 70 beats /min. A pelvic binder was in place. The FAST exam in the trauma bay was negative.
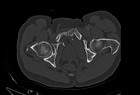
Review of the CT scan confirmed the diagnosis of a covered aortic rupture at the transition zone between the aortic arch and the descending aorta (Fig 1 and Fig 2). At the level of the pelvis, the patient suffered a fracture of the upper and lower pubic ramus bilaterally as well as a fracture of the sacrum on the right side (Fig 3 and Fig 4).
The patient was transferred to the hybrid OR, where a bypass (PTFE, 8mm) from the left common carotid artery to the left suclavian artery was performed. An aortic stent (Medtronic, Valiant Thoracic, Santa Rosa, CA, USA) was then introduced through the femoral artery and placed over the rupture site, occluding the outflow to the left subclavian artery (Fig 5 and Fig 6). The patient tolerated the procedure well, so that osteosynthesis of the pelvis could be performed immediately following the vascular repair. The pelvis was fixated using a plate at the symphysis for closure of the anterior pelvic ring and an iliosacral screw for fixation of the right sacrum fracture and posterior pelvic ring (Fig 7).
The further postoperative course was uneventful and the patient was transferred to a regional hospital eight days postoperatively. Two weeks after the accident he was discharged from hospital.
Discussion
Symptoms and clinical findings:
Symptoms for a traumatic aortic rupture can be very vague, so a high index of suspicion is required. Aortic rupture is a frequent cause of death in severe blunt trauma. Usually it is a result of rapid deceleration in high speed accidents or falls from heights. Many of these patients die at the scene. Thoracic pain, dyspnoea or dysphagia may indicate aortic injury. However, in the setting of a polytraumatized patient, these symptoms are not sensitive or specific at all.
More specific clinical findings for an aortic rupture may be a cardiac murmur, hoarseness, a left subclavian haematoma, a bilateral femoral pulse deficit or Horner’s syndrome. Thoracic or abdominal steering wheel/seatbelt imprints on the skin indicate significant injury and should awake the suspicion of an aortic injury. In patients with a widened mediastinum, and/or an abnormal aortic contour in the chest X-ray, possibly in combination with a haemothorax, an aortic injury should be excluded.
Unfortunately, absence of these clinical and basic radiological signs does not exclude an aortic injury. However, the presence of one of these findings must lead to further diagnostic workup, including a contrast enhanced angio-CT scan, which has been shown to have the best diagnostic accuracy. The case presented impressively that a patient without any of the above mentioned symptoms and unremarkable clinical examination can suffer from a traumatic aortic rupture.
Epidemiology:
A study analysing the US national trauma database showed an overall incidence of blunt aortic injuries of 0.3% in trauma patients admitted to US hospitals. Since injuries to the aorta have a high potential to lead to death at the scene, this number may underestimate the actual incidence, as many patients will never be correctly diagnosed and are not included in statistics.
Most of the patients with traumatic aortic injuries have significant concomitant injuries: 31% suffer major head injuries, 29% major abdominal injuries, 15% pelvic injuries. The mean Injury Severity Score (ISS) in patients with blunt aortic injuries was reported to be 40. Overall mortality after admission to hospital was reported to be up to 55%.
Management:
Initial treatment should include resuscitation with a slightly low systolic blood pressure (about 90mmHg), with antihypertensive medication if needed. In severe multitrauma patients or elderly patients, non-operative treatment for minor aortic injuries may be applied. However, surgical or endovascular stent repair should be considered in younger patients.
Options for the treatment of traumatic aortic rupture include open surgical repair of the affected segment of the aorta or the newer TEVAR (Thoracic Endovascular Aortic Repair) technique. The advantages and disadvantages of these two techniques will not be discussed in detail here. However, it is important that surgical trauma is less with the TEVAR technique and therefore the “second hit” is smaller, which is a significant benefit for heavily traumatized patients.
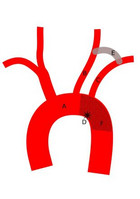
With the TEVAR technique, the ruptured aortic segment is covered from the inside, by placing a stent that is introduced over a femoral arterial access. Since most of the traumatic aortic ruptures are located just distally to the left subclavian artery (90%), stenting of these lesion also means occlusion of the left subclavian artery. Therefore bypass from the left common carotid artery to the left subclavian artery is performed prior to the stenting of the aorta, in order to preserve blood flow to the subclavian artery. Moreover, a vascular plug was placed at the origin of the left subclavian artery in order to avoid backflow and an endoleak. In Figure 5, the vascular situation after the TEVAR procedure is sketched (A: arch of aorta, B: left common carotid artery, C: left subclavian artery, D: aortic injury, E: bypass B to C, F: aortic stent). Video 1 shows the 3D reconstruction of the CT scan after the TEVAR procedure.
Conclusion
Aortic rupture as a result of blunt deceleration trauma is a rare condition and requires a high index of suspicion from the managing trauma team. Once diagnosed, systolic blood pressure should be kept low at approximately 90mmHg – if necessary by the administration of antihypertensive medications. Definitive treatment is a multidisciplinary approach including open cardiac surgery or interventional endovascular aortic repair techniques.
Selection of recommended articles
Antonopoulos CN, Sfyroeras GS, Kallinis A, Kakisis JD, Liapis CD, Petridou ET. Epidemiology of concomitant injuries in traumatic thoracic aortic rupture: A meta-analysis. Vascular. 2014 Jan 23.
Arthurs ZM, Starnes BW, Sohn VY, Singh N, Martin MJ, Andersen CA. Functional and survival outcomes in traumatic blunt thoracic aortic injuries: An analysis of the National Trauma Databank. J Vasc Surg. 2009 Apr;49(4):988-94.
Pongratz J, Ockert S, Reeps C, Eckstein HH. [Traumatic rupture of the aorta: origin, diagnosis, and therapy of a life-threatening aortic injury]. Unfallchirurg. 2011 Dec;114(12):1105-12.
Schulman CI, Carvajal D, Lopez PP, Soffer D, Habib F, Augenstein J. Incidence and crash mechanisms of aortic injury during the past decade. J Trauma. 2007 Mar;62(3):664-7.
Sastry P, Field M, Cuerden R, Richens D. Low-impact scenarios may account for two-thirds of blunt traumatic aortic rupture. Emerg Med J. 2010 May;27(5):341-4.
Steuer J, Wanhainen A, Thelin S, Nyman R, Eriksson MO, Björck M. Outcome of endovascular treatment of traumatic aortic transection. J Vasc Surg. 2012 Oct;56(4):973-8.
Jakimowicz T, Rowiński O, Gałązka Z, Solonynko B, Szmidt J. Endovascular repair of traumatic thoracic aortic rupture: a single centre experience. Kardiol Pol. 2013;71(12):1273-8.
Mirhosseini SM, Asadollahi S, Fakhri M. Surgical management of traumatic rupture of aortic isthmus: a 25-year experience. Gen Thorac Cardiovasc Surg. 2013 Apr;61(4):212-7.





Comments